An Overview of How Immunotherapy Is Used to Treat Cancer
Immunotherapy is a modern approach to cancer treatment that focuses on supporting the body’s own immune system in recognizing and responding to cancer cells. This article explains the basic principles behind immunotherapy, the different ways it is used in clinical practice, and how it differs from more traditional cancer treatment methods.
How Immunotherapy Works in Cancer Treatment
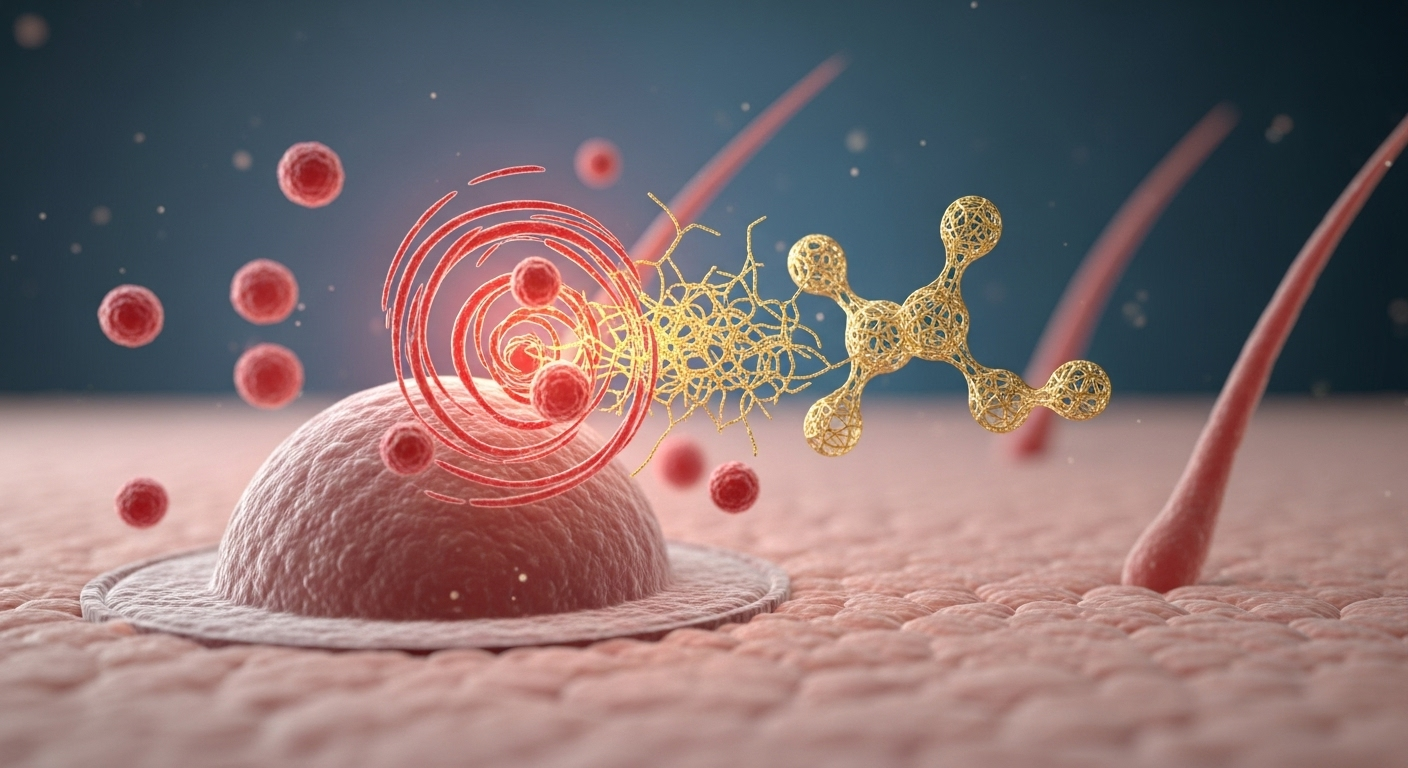
Immunotherapy functions by stimulating or enhancing the immune system’s capacity to identify and eliminate cancer cells. The immune system naturally patrols the body for abnormal cells, but cancer cells often develop mechanisms to evade detection. Immunotherapy medications work by blocking these evasion tactics or by providing the immune system with additional tools to recognize cancer markers. Some treatments use checkpoint inhibitors that remove the “brakes” on immune cells, allowing them to attack cancer more aggressively. Others introduce engineered immune cells or antibodies specifically designed to target cancer cell proteins.
The treatment process typically involves intravenous infusions administered in clinical settings over several weeks or months. Patients receive regular monitoring to assess treatment response and manage potential side effects. The immune system’s enhanced activity can sometimes cause inflammation in healthy tissues, requiring careful medical supervision throughout the treatment course.
Types of Cancer Immunotherapy
Several distinct categories of immunotherapy exist, each targeting different aspects of immune function. Checkpoint inhibitors represent one of the most widely used types, blocking proteins like PD-1, PD-L1, or CTLA-4 that normally prevent excessive immune responses. Monoclonal antibodies are laboratory-created proteins that bind to specific cancer cell markers, either directly destroying cells or marking them for immune system destruction.
CAR-T cell therapy involves extracting a patient’s T-cells, genetically modifying them to better recognize cancer, and reinfusing them into the body. Cancer vaccines work by exposing the immune system to cancer-associated antigens, training it to recognize and attack similar cells. Cytokine therapy uses proteins that naturally regulate immune responses to boost the system’s cancer-fighting capabilities.
Adoptive cell transfer represents another approach where immune cells are removed from tumors, multiplied in laboratories, and returned to patients in larger numbers. Each type offers unique advantages depending on cancer type, stage, and individual patient factors.
Immune System and Cancer Interaction
The relationship between the immune system and cancer involves a complex interplay of recognition, evasion, and adaptation. Healthy immune surveillance continuously monitors for cellular abnormalities, including early cancer development. However, cancer cells can develop sophisticated methods to avoid immune detection, including reducing the expression of recognition markers or secreting substances that suppress immune responses.
Tumor microenvironments often create immunosuppressive conditions that protect cancer cells from immune attacks. Cancer cells may also mutate rapidly, changing their surface proteins faster than the immune system can adapt. Some cancers exploit immune checkpoints, natural regulatory mechanisms designed to prevent autoimmune reactions, using them as shields against immune responses.
Immunotherapy aims to overcome these evasion strategies by either enhancing immune recognition capabilities or removing the barriers that cancer cells create. Understanding these interactions helps medical professionals select the most appropriate immunotherapy approaches for specific cancer types and patient situations.
Immunotherapy Compared to Traditional Cancer Treatments
Traditional cancer treatments like chemotherapy and radiation therapy work by directly damaging or destroying cancer cells, often affecting healthy cells in the process. These treatments typically produce immediate, measurable effects but may cause significant side effects due to their non-selective nature. Immunotherapy offers a more targeted approach by training the body’s natural defenses to specifically attack cancer cells while generally sparing healthy tissue.
The timeline for immunotherapy responses often differs from conventional treatments. While chemotherapy may show rapid tumor shrinkage, immunotherapy responses can develop more gradually as the immune system builds its anti-cancer response. However, immunotherapy responses may prove more durable, with some patients experiencing long-term remission even after treatment completion.
Combination approaches increasingly show promise, with immunotherapy used alongside traditional treatments to enhance overall effectiveness. The side effect profiles also differ significantly, with immunotherapy potentially causing immune-related adverse events rather than the typical chemotherapy side effects like hair loss or severe nausea.
| Treatment Type | Mechanism | Response Timeline | Duration of Effect |
|---|---|---|---|
| Chemotherapy | Direct cell destruction | Days to weeks | Treatment-dependent |
| Radiation Therapy | DNA damage to cancer cells | Weeks to months | Localized, permanent |
| Immunotherapy | Immune system enhancement | Weeks to months | Potentially long-lasting |
| Surgery | Physical tumor removal | Immediate | Permanent if complete |
The integration of immunotherapy into standard cancer care continues evolving as researchers better understand optimal timing, combinations, and patient selection criteria. Many oncologists now consider immunotherapy as a first-line treatment option for certain cancer types, while others reserve it for cases where traditional treatments have proven insufficient.
Immunotherapy has transformed cancer treatment by offering a fundamentally different approach that works with the body’s natural defense mechanisms. While not effective for all patients or cancer types, it provides valuable treatment options that can complement or sometimes replace traditional therapies. As research continues advancing, immunotherapy applications are expanding, bringing hope to patients facing various cancer diagnoses. The field’s rapid development suggests that future cancer treatment will increasingly rely on personalized approaches that combine multiple treatment modalities for optimal outcomes.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.




